It’s tick time… and ticks, including those that carry Lyme disease, are in long grass and on bushes, waiting to grab onto you, your clothing or your pet as you pass by.
The numbers of cases of Lyme disease are increasing – the US Center for Disease Control (CDC) estimates over 300,000 cases occur each year, although only around 30,000 are reported. Lyme infected ticks are present in largest numbers in north eastern US but, with global warming and increases in deer population, deer and the ticks they carry, are migrating north and are now found in parts of Canada as well. They are even found as far south as Florida, but are less likely to contact humans in warmer climates, as they hide during the day to seek shelter from the heat.
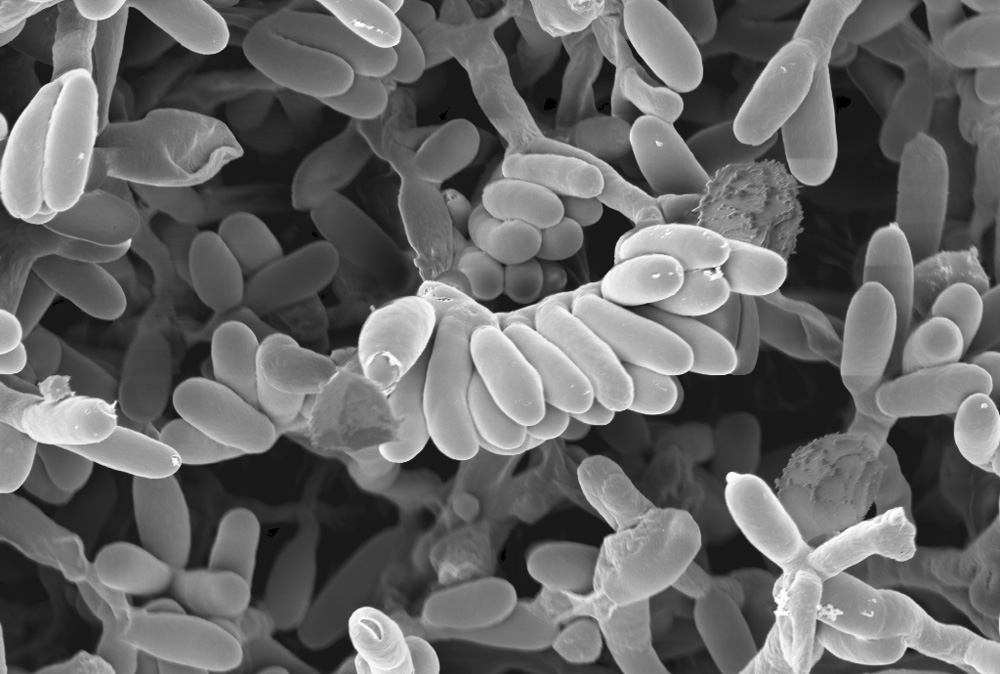
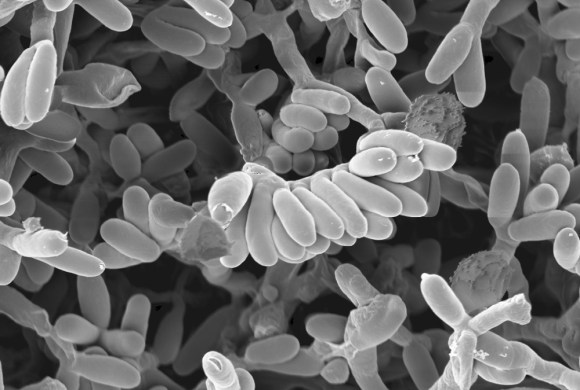
Lyme disease is caused by bacteria in the Borrelia family – tests look specifically for the Borrelia bergdorferi – but some researchers suspect that all bacteria in the Borrelia class can cause similar disease. The bacteria are carried mainly by black-legged ticks, also called deer ticks or bear ticks, and these ticks in turn are carried by deer, mice, gray squirrels, opossums and chipmunks. Lyme disease is not something new – DNA from the bacteria that causes it was identified in the 5,300 year old bones of Ötzi the Iceman, a mummy found in the Eastern Alps in 1993.
Early symptoms of Lyme disease include fever, chills, headache, fatigue, muscle and joint pain, and swollen lymph nodes. 70 to 80% of people who are infected get a rash that gradually increases in diameter over several days, and about 30% of these have a distinctive “bulls eye” appearance. The rash can get as large as 30cm (12 inches) across, most often is uniformly red or bluish red, and is rarely itchy of painful. However, 20 to 30% of infected people have no rash as all so its presence is not necessary for a positive diagnosis.


Diagnosis of Lyme disease is usually made by symptoms plus a history of tick exposure. However, immature ticks are tiny and flesh coloured, and can be difficult to see on the skin. Blood tests look for antibodies to the bacteria, not for the bacteria itself, as Borrelia dislike oxygenated environments and leave the blood quickly for other less oxygenated tissues, such as joint fluid or bone. As antibodies take several weeks to develop, blood tests will often not show positive results in the first few weeks of an infection. All of this suggests that many cases are not readily diagnosed.
If diagnosed and treated early, however, a full recovery is likely. It is treated with antibiotics, usually amoxicillin, tetracycline, doxycycline or cefuroxime, generally for 10 to 21 days but sometimes longer.

Ticks are tiny – the size of a poppy seed – so you need to look carefully to see them. As they feed, they become engorged with blood, becoming larger and easier to see. But you want to remove ticks as soon as possible. The tick must attach to skin for 24 hours to transmit the disease, so early removal can reduce the chance of infection. Check skin carefully after walking in tall grass or gardening – ideally, remove all clothing first so you can check all areas of your body. Be aware that clothes and pets can carry ticks too, that can bite you later, so handle clothing carefully (best with rubber gloves if you suspect ticks are present). Place clothes in the dryer at high heat for at least 15 minutes – dry first to kill any ticks, then wash later! Ticks have been reported to survive washing of clothing.
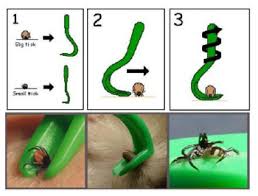
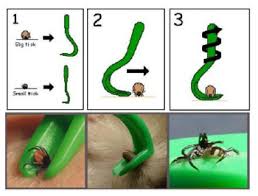
There are two good techniques for tick removal, depending on what tool you are using:

-
Fine-tipped tweezers – grasp the tick close to the skin. You want to grip the head, not the body (squeezing the body can cause the tick to regurgitate infected fluids into the bite, increasing the risk of infection). Pull straight upwards (or in the direction opposite to the angle of entry of the mouth parts, if you can see this), and pull slowly and steadily. Don’t twist or jerk the tick out quickly as this can increase the chance of the head or mouth parts breaking off and staying in the skin. Any parts left in the skin will also cause irritation and can increase the risk of other infections and can be removed as you would remove a splinter, with tweezers or a needle. Don’t use flat-tipped tweezers to remove ticks, as these will squeeze the body, increasing the chance of fluid regurgitation.
-
Tick removal tool (O’Tom Tick Twister is one recommended brand I found) – slide the tool between the body of the tick and the skin, and rotate the tool 2 to 3 times until the tick detaches. Rotate in only one direction to decrease the risk of breaking off mouth parts. Follow included instructions carefully.
Ticks are also more likely to regurgitate fluids into the wound, increasing the risk of infection, if they are irritated. Tick removal techniques that involve burning, freezing or using harsh chemicals to make the tick let go are not recommended. A viral internet video showing a technique using liquid dish detergent and a cotton ball seems to be effective at removal, but the irritating soap may increase the chance of fluid regurgitation. This technique is not recommended in the sources I consulted, due to a lack of testing to ensure the risk of regurgitation is not increased.
Ticks can be crushed in a tissue then flushed, or encased in a piece of adhesive tape. Placing into a ziplock baggie is another option. Some sources suggest keeping the tick for confirmation testing, in case symptoms of Lyme disease develop in the future.
So, pop a pair of pointed tweezers or a tick removal tool into a baggie and add it to your hiking or gardening equipment this summer! If you have room, add a roll of adhesive tape to safely remove any unattached live ticks you see on your skin, clothing or pet. And check your skin carefully after enjoying an outing in long grass or bushes where ticks may be waiting for you, so you can remove them before any infection has a chance to take hold…
Have you had a tick bite? How did you handle it? Leave a comment below!
References: WebMD.com; PetMD.com; http://www.bada-uk.org/correct-tick-removal