I know, I know… we’re all tired of hearing about it. Won’t COVID ever go away? **sigh** Instead of settling into a flu-like seasonal pattern, this virus has taken on a life of its own and refuses to behave like most viruses.
How COVID-19 is different
An article in The Conversation newsletter this morning discussing a new study of people in nursing homes – a vulnerable population we need to protect – caught my attention. Surprisingly, those who had been infected with the BA.1-2 strain were 30 times more likely to catch the BA.5 strain that followed it a few months later. This is the opposite of what is expected – usually, catching a virus improves resistance to infection approximately as well as getting a booster shot (just a riskier way to develop immunity). This virus continues to surprise researchers…
If this applies to all ages (and chances are, it does), this means that the protective practices we all know so well –handwashing, distancing, and masks – are important again. The medical community is already reporting an uptick in cases here in Canada this summer, and school hasn’t started yet. In communities south of the border, where kids are already back to class, some schools have already cancelled classes to try to control the spread.
And, rather than settling into a predictable seasonal pattern like the ‘flu, it seems to surge in late summer, just as the kids are heading back to close quarters in school where bugs are passed around more easily.
COVID also is good at hanging out in our bodies long after we should have recovered — something rarely seen with other common respiratory viruses. Researchers report that 1 in 10 will continue with disabling symptoms from the infection for months to years in the form of Long COVID. This is a huge future concern for our healthcare systems.
Metformin… wonder drug?
Another interesting study I read on the subject of COVID, was that the diabetes medication, Metformin, can reduce the chance of developing Long COVID by 43% if taken early in the onset of the acute infection. I have to admit, my greatest fear beyond the risk of having a severe infection (for which I never miss a booster!) is getting Long COVID.
Metformin, by the way, may just become the wonder-drug of the century, from what I’ve been reading about it recently. As well as improving insulin sensitivity (its main use), it’s been found to reduce the risk of relapse of certain cancers and appears to promote longevity, according to preliminary research. People with Type 2 diabetes who take Metformin statistically live longer than people who don’t have diabetes!
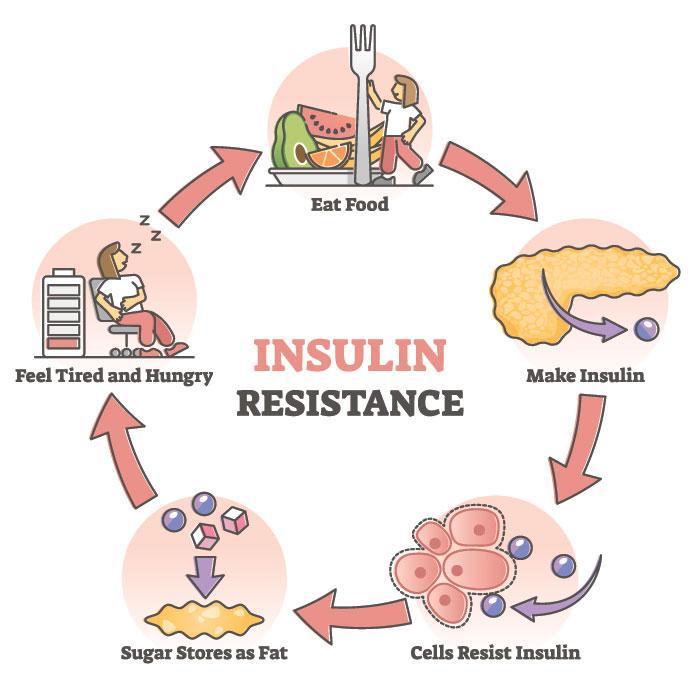
Type 2 diabetes develops when insulin stops working as it should – the body becomes resistant to the effect of the insulin hormone (called “insulin resistance”) and, in response, the pancreas produces more insulin to keep blood sugar normal. This compensation can continue for years – some estimate that insulin resistance can start as long as 10 years before sugar in the blood (“blood glucose”) starts to rise.
It astounds me that doctors still only look at blood sugar, even though blood insulin measurement is a relatively inexpensive test. My doctor told me that they don’t do this test (that would detect the development of diabetes years sooner) because there was no “protocol” for it! Why isn’t there a protocol for a simple test that would diagnose a serious disease like diabetes years sooner??? This is a prime example of one of the biggest problems in medicine – “knowledge translation”, getting what has been learned through research into real-world practice. It takes, on average, 17 years for an important medical discovery to become routine practice for doctors. Old habits are hard to change, and it takes time for practice guidelines and protocols to be re-written and put into practice. Like all of us, medical professionals need to be educated about new ways of doing things and then need to actually change their way of doing things. You know about old dogs learning new tricks. But I might be ranting again, am I???
And the new vaccine…
Another factor against us as fall approaches, is that the newest version of the COVID vaccine – the updated one that’s strongly recommended – won’t be available for several weeks, probably November here in New Brunswick, my pharmacist told me. And he’s not sure he’s going to offer it, as it increases his workload incredibly and, at the same time, compensation for giving the shot has tanked… so won’t be financially feasible for many pharmacists. It’s hard to hire extra staff when you’re making almost half as much as last year for each injection given, while salaries have gone up. This may mean that shots will be harder to access than before.
The epidemiologists are predicting a late-summer “COVID wave”, so it’s looking like there will be a gap in protection for many people.
Time to think about digging out those masks and hand-sanitizers again…
Actually, I’m still finding masks tucked into purses and coat pockets, so I don’t have to dig too far, but I’ve started feeling a little silly wearing one again, much like I did back in early 2020. We seemed to be the only ones who were wearing one then… and they were homemade since the commercial ones were being reserved for medical workers. I’ve since upgraded to N95s, of course.
I still have my little spray bottle of hydrogen peroxide to sterilize my masks too, sitting on my buffet. Hydrogen peroxide, used as a steam after each use, has been shown to sterilize masks well enough for hospital re-use up to 30 times, so we know peroxide kills COVID and doesn’t damage the mask. When coupled with rotating masks so they’re only worn every 3 to 4 days (also known to kill off the virus) I feel safe re-wearing masks until they are obviously soiled. I’m hoping someone will test this cleaning method but, until then, I’ll keep my 4 masks lined up, spraying each after wearing it, and putting it at the back of the line, as this is the best practical method of sanitizing I know of!
So, how about you? Will you be going back to masking and hand-washing, with cooler weather and classes keeping people indoors, or are you going to just take your chances when you’re in crowded places??? It’s time to think about it…
References/Additional Reading:
COVID-19 boosters are the best defence — The Conversation
“Breakthrough” study: Diabetes drug helps prevent long COVID — Medscape
Outlive – Dr. Peter Attia (check your local public library for availability)
Lifespan – Dr. David Sinclair (longevity researcher at Harvard Medical School). Available through the public library system.
One in five doctors with Long COVID can no longer work: Survey — Medscape
Stay tuned for a future blog on longevity! And, just a reminder, the ads you see here are sponsored by my web hosting site, WordPress, and not endorsed by me! (The price to be paid for a free website these days…) jcb