Just days after arriving in Florida, hurricane Matthew began its advance up the coast. A category-4 hurricane was a new experience for my husband and me…what should we do? Stay or go? This was a frequent topic of conversation with neighbours, even those we didn’t know…
We decided to take the safe route and flee, but what to do with a fridge full of food when we returned? I learned from others how to reduce health risks from spoiled food after you get back…unfortunately, most of it only after the storm, although ideally some preparation should have been done before leaving.
Many of these tips would apply to any power outage situation, so I thought I’d share these with you…
The best approach is to start preparing at the first warning of the approach of a storm. Turn down the settings of both fridge and freezer so you are starting with a lower temperature – a cooler refrigerator and deeper freeze will last longer when the power goes out.
Frozen jugs or ziplock bags of clean water will work as ice packs in the fridge and freezer, maintaining the coolness and, at the same time, eliminating air space. We know that heat rises and cold air falls, so filling up the dead space will reduce the air exchange that occurs each time the door is opened.
These frozen bottles and bags will also provide clean drinking water later if needed. Often tap water is deemed unsafe for several days after power is restored while the system is flushed, especially in warmer climates… This is not such a worry in Canada, where most power outages occur in the winter, but for those of us in rural areas with our own water supply, no power means no pump and no water!
Next, you want to pack your foods closely together to mimic how they would be packed in a cooler, rather than being nicely spread out on the shelves. Just as a block of ice takes longer to melt than smaller chunks, a block of tightly packed foods will stay frozen or cool longer, especially if surrounded tightly by ice packs, creating a “cooler” within your fridge.
It’s relatively easy to determine how long the power was out, especially if you are able to stay at home, but it can be more difficult to know how long the food in your refrigerator stayed cold or frozen.
The rule of thumb you will find on government websites is: food will stay cold in an unopened refrigerator without power for at least 4 hours, frozen food in a full freezer for up to 48 hours and in a half-filled freezer for about 24 hours. That being said, a lot depends on the quality of the refrigerator and how the food is packed into it.
The ideal way to monitor the fridge temperature is with a probe thermometer similar to those often used in cooking these days. An ordinary fridge thermometer inside the fridge will tell you the temperature but you need to open the fridge to see it, allowing cold air to escape each time you do this…definitely not recommended if the power is out! Checking the temperature after the power is back is helpful if it’s still below the recommended 5C (40F), but if the temperature is higher you have no way to know how long it’s been out of the safe zone.
A “min/max” thermometer, used for storage of critical items such as vaccines, has a probe (sometimes wireless) that is placed inside the fridge, while the thermometer itself remains outside where it can be read without opening the fridge door. It records the minimum and maximum temperatures and the times that these occurred. It can also be set with the desired temperature range sounding an alarm and noting the time that the temperature left this range…valuable information if you have to leave home during the storm. Like many electronics these days, prices of these units are dropping and can be found for under $100 (I found one for $35CDN for my vaccine storage!). It might be worth the investment if you lose power often and end up discarding food because you don’t know if it is safe.
A simple tip, however, which I learned from a hurricane-savvy friend, is to freeze a glass of water and place a coin on top. If the water thaws then refreezes before you return, the coin will no longer be sitting on top of the ice. If it is halfway down, your ice was partially thawed then refrozen; if it is at the bottom, then it is likely that your food, like the ice in the glass, completely thawed before the power came back on. Nice trick!
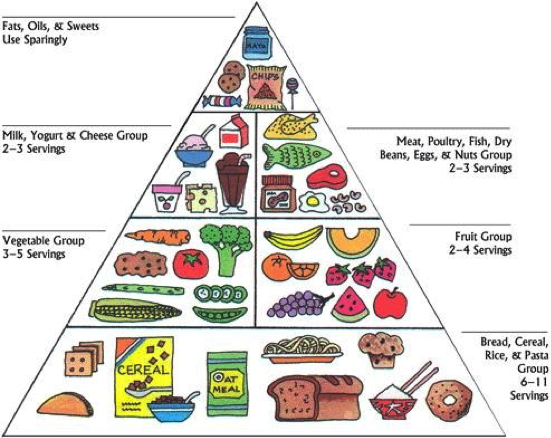
Some foods are more likely to spoil than others. These include meats, dairy, eggs and leftovers. It is suggested to remove these from the refrigerator and store them in a cooler packed with ice. This system is easier to monitor and the ice can be replaced as it melts, extending the life of the food. If you’re in a cold climate, it is recommended to freeze water outdoors to restock your cooler, rather than actually putting the cooler outside – sunshine can warm the food even if it is below freezing outside, and animals can also be attracted to the food.
Be aware that juices from meat can contaminate other foods – store separately or in leak-proof packaging. As a general rule, store foods that will not be cooked before eating above meats and fish in the refrigerator so juices cannot drip onto them, potentially causing contamination.
Government sites suggest that food poisoning occurs in 1 person in 8 each year… Never taste food to determine if it is spoiled. When in doubt, throw it out!
If you are interested in more detail, including a list of stability of various foods, check out this site: http://www.fsis.usda.gov
We survived the experience with no damage to our condo and only minor damage to our boat. But it is so sad to see many others who did not fare so well, and it was stressful just worrying about what might happen. I think I’d take a good old Canadian snowstorm over a hurricane any time!