Falling when you’re a child is part of life but falling as an adult puts you at risk of an injury, whether you’re in you’re 20’s or your 80’s. There are strategies to prevent falling but, if you do fall, you can also fall “well”…

Here’s my story: while excitedly trying to book concert tickets on my phone and climbing the stairs, I took a step backwards to say something to my husband, missed the stair, and landed with full weight on a turned ankle. The bad sprain that resulted required several weeks recovery (including an air cast) plus weeks of physiotherapy… all from a moment of inattention.
Of course, much of what I want to discuss is common sense. However, many falls are due to not paying attention or neglecting to correct an obvious hazard. Taking a few moments now may mean you will avoid an injury that could take weeks to recover from.
If you do fall, of course you’ll only have a fraction of a second to react… but falling properly can decrease your chance of a serious injury. Here are some suggestions that may help you to react correctly:
-
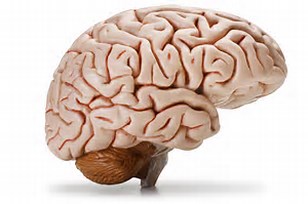
Protect your head – It’s the most important part of your body!
-
If falling forward, turn your head to the side to protect your nose and mouth. Bring your arms up in front. Think of landing in a push-up, with arms flexed to absorb the impact.
-
If falling backward, round your back and tuck your chin to your chest.
-
-
When falling sideways, turn as you fall if possible. Try to land on the “meaty” area of your butt to cushion your fall rather than land directly on your hip.
-
Keep arms and legs bent and stay loose to absorb impact.
-
Try breathing out as you fall to keep relaxed.
-
Try to break your fall using both the hand and forearm to avoid excess force on the wrist.
-
Roll with the impact if you can to reduce the force on one area of the body.
-
Here is a site with more suggestions on falling “well”: http://www.wikihow.com/Fall-Safely
Of course, it’s always best to avoid a fall that could cause a painful injury. Most falls are preventable — being aware of the possibility and taking preventative action could prevent a lot of pain:
-
Exercising regularly to maintain flexibility and balance may help you to prevent a fall.
-
Physical activity builds strength, coordination and balance. Slow, gentle exercise like yoga or Tai Chi is very effective. For those who are less able to exercise, even exercise done while sitting in a chair can improve muscle strength, improving the ability to maintain balance when standing. There are lots of exercise programs on the internet – sparkpeople.com is a free one that includes a series done in your chair for elderly or those with a disability.
-
Stretching regularly can improve flexibility, giving increased range of movement and reducing chances of pulling a muscle if you do slip or fall. Stretches can easily be done in bed when you awaken or before going to sleep. Stretching can also be beneficial for muscle spasm related problems, like low back pain or heel pain. Consult a physiotherapist or massage therapist for personalized exercises if you have specific problems.
-
-
Around the home
-
Footwear – Floppy slippers, sock feet, high heels, or slick soles are best avoided. Choose footwear with non-slip soles whenever possible.
-
Stairs – Always use handrails, and pay attention to your footing when climbing or descending stairs. Ensure stairs have a slip resistant covering.
-
High traffic area – Keep clear of tables, lamps, etc.
-
Remove hazards – Ensure rugs are non-slip, carpet edges are secure, and electrical wires are securely wrapped up and tucked away. Clean spills of liquids, grease, powders or food right away.
-
Lighting – Have adequate lighting to ensure you can see potential hazards at night, especially on stairs. Have a lamp within reach of your bed in case you need to get up at night. Ensure a clear path to switches that are not near the door of the room. Keep a flashlight in an accessible area (that you will remember!) in case of a power outage.
-
-
Use proper safety equipment, indoors and out
-
If you need to use out-of-reach storage area, have a sturdy folding ladder available – never stand on furniture to reach high areas.
-
Ensure your bath tub has a properly installed non-slip surface. Elderly or disabled should consider installing safety hand rails, but and using a bath chair with handheld shower for increased safety.
-
-
If you’ve had a fall that is not easily explained, make an appointment with your doctor or pharmacist to discuss possible causes:
-
Check medications – some medications can increase the risk of falling. Check type, dosage and number of drugs being taken.
-
Check health conditions – some falls are caused by an undiagnosed health problem that can be corrected.
-
Review any history of falls to identify potential problems.
-
If you have a chronic disability, an occupational therapist may be able to provide you with solutions that will improve your lifestyle and reduce risk of injury.
-
Lastly, just paying attention to what you are doing can often prevent injuries. Certainly, my fall on the stairs was completely due to not paying attention to what I was doing. It’s easy to run on “autopilot” as we perform routine activities, but so important to always remain aware of our surroundings …All just common sense, of course, but worth some conscious thought!
Do you have other ways to prevent falls, or to prevent injury if you do fall? Leave a comment below!
Reference: Mayo Clinic website.