The avoidable underlying problem of many chronic diseases
Infographic credit: BreatheWellBeing.in
What if you could lower your risk of a slew chronic diseases, like heart disease, diabetes, cancer, inflammatory diseases, and perhaps even Alzheomer’s, just by making some changes to your diet and lifestyle… giving yourself extra healthy years to enjoy life? Would you do it? Would it be worth the effort? New research suggests reversing “insulin resistance”, through improvements in diet and adding some exercise, could prevent many diseases from developing and possibly reverse some at early stages. And if you make these changes one little step at a time, they can be easy to do!
What is insulin resistance?
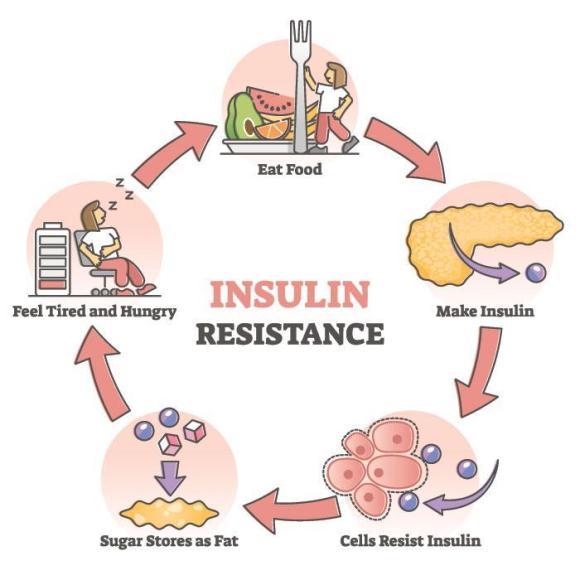
You may be familiar with the term “Insulin resistance” … it’s understood to be the first step in the development of diabetes and, more recently, it’s been strongly suggested as the underlying problem driving many other chronic conditions too. Insulin is a hormone needed to enable sugar/glucose (as well as other nutrients) to get into our bodies’ cells. Being resistant to insulin means that, although the insulin-producing beta cells in your pancreas are able to produce the hormone, your cells are not responding as they should. Your pancreas is able to produce extra insulin for a long while to compensate (resulting in higher-than-normal blood insulin, while blood sugar remains normal) but, eventually, it can’t keep up and your blood sugar will begin to rise. At this point regular blood testing will pick up the problem and you will be diagnosed with pre-diabetes or diabetes (depending on how high your sugar level is). However, the insulin resistance has likely been in progress for years by the time this happens. (Note that “developing insulin sensitivity” is essentially the same thing as “reducing insulin resistance”.)
But insulin resistance (or a lack of insulin sensitivity) also drives cholesterol problems, weight gain (especially around the waist), bloating, fatigue, food cravings, mood swings, irritability, needing to urinate at night, and feeling hungry/unsatisfied after eating. Other symptoms include non-alcoholic fatty liver disease (from all the extra sugar being stored there as fat), inflammation, sleep apnea, slow metabolism, loss of muscle mass, acne, low testosterone, poor focus, and increased response of the sympathetic “fight or flight” system to stress. Increased insulin also raises your blood uric acid, the substance that can cause gout or kidney stones when it becomes too high to stay dissolved in the blood. These are all symptoms that you may be developing a problem with responding to insulin. Quite a list, right?
How do you test for Insulin Resistance?
Unfortunately, although there is a simply way to detect insulin resistance, few doctors do this. The result is, by the time it’s diagnosed, you may already have problems with high cholesterol, high blood pressure, excess weight gain around the middle. Along with the diabetes diagnosis, this collection of abnormalities is known as “metabolic syndrome” and it puts you at risk for heart disease and stroke, as well as other chronic diseases. And, although it all could have been corrected by a few diet and lifestyle changes years before, you’ll likely be prescribed several medications to treat the cholesterol, blood pressure, and diabetes, and will be told to exercise to lose weight (and you’ll probably have a hard time getting the weight off!)
But to detect insulin resistance long before this happens, your doctor simply has to order a fasting blood insulin test along with the fasting blood glucose they are probably already doing. There is a simple calculator available online, called the HOMA-IR calculator, that you can easily find using Google. HOMA-IR stands for Homeostatic Model Assessment for Insulin Resistance, and it looks at the relationship between fasting glucose and fasting insulin. You just plug in the 2 numbers and it gives you the result, along with an interpretation of what the result means. It was so easy, I have difficulty understanding why my doctor wasn’t doing it, especially given the damage that high insulin can cause over time. She actually wasn’t sure whether our provincial Medicare would pay for the test but was willing to try (unlike my hubby’s doctor, who stated it wasn’t covered and refused to order the test.) I guess she’d never asked for the test to be done before, but I was pleased she was willing to try.
PS, the test was covered, and I was surprised by my result… and motivated to change! Insulin resistance explains the kidney stones I’ve had in the past couple of years, as well as the gradual weight gain that I’ve struggled to avoid, and had difficulty to correct in spite of using a strict keto diet for the past 8 months. I dove into researching how to correct insulin resistance, of course, and found plenty of safe, fairly easy-to-do changes I could make. So, I thought I’d share what I learned with you!
How to improve insulin sensitivity
First, of course, is exercise. Any exercise will help, but studies suggest that adding resistance training (i.e. weights) is an important addition to fight insulin resistance, and exercise later in the day has a greater effect than that early in the morning. But even small increases in exercise, like taking the stairs instead of an elevator) can help (I say as I sit at my desk… I’ll be sure to go for a walk when I finish!)
Intermittent fasting, which involves reducing the hours during the day when you eat, can help too. Doctors recommend fasting for 16 hours a day, which simply means keeping your food intake within an 8-hour window each day. They usually recommend shifting gradually to this pattern of eating, for example, reducing to 12 hours at first then compressing your food intake by an hour at a time. It can also be done by keeping total food intake less than 600 calories on 2 non-consecutive days each week, but that sounds rather unpleasant to me! (Don’t think I could do that…)
Decrease inflammation by fasting (as above) and ensuring you are getting enough vitamin D. Here in Canada, the sun isn’t strong enough from October to April, so we need to supplement or spend the winter somewhere warm and sunny! When the sun shines on our skin, it converts cholesterol into vitamin D, creating thousands of units a day, depending on several factors, like the amount of skin exposed, sunscreen use, and the amount of natural pigment in the skin. When supplementing, you’d want to take at least 1000 units of the vitamin, and up to 2000 iu a day is considered very safe. Here’s a link to a blog I wrote in 2018 about Vitamin D if you’d like to know more…
Newer research into gut microbiome (your gut’s natural bacteria/yeast/virus contents) suggests it may have an influence on inflammation as well. Addressing any digestive problems you may have is a good start to being healthier overall.
If you’re often stressed-out, decrease your stress response (and therefore stress hormones, like cortisol) by using stress-reduction techniques such as yoga, tai chi, or meditation. Listening to or playing music, and making art can also lower stress. Note that stress hormones raise your blood sugar to provide energy for dealing with the stressful event.
Work to improve your sleep, if you don’t sleep well at night. A good night’s sleep can lower your stress hormones. PS you won’t be eating if you’re asleep (so it helps support intermittent fasting!)
Eat more veggies and fiber. These foods support healthy gut bacteria that will produce a substance called butyrate, known to help improve insulin sensitivity. Fiber also slows the rate of absorption of sugar and other carbohydrates, preventing spikes in blood sugar that stimulate lots of insulin production. If you have digestive problems, you might consider taking a probiotic capsule (and/or eating more probiotic fermented foods) to improve your gut flora, the blend of good bacteria in your intestines. Nuts and seeds are very high in fiber and make good snacks, if you’re looking for something to substitute for sweet treats!
Add some herbs to your food. Garlic, ginger, turmeric, and cinnamon can help improve insulin sensitivity and reverse the trend toward insulin resistance. Green tea, and the minerals Chromium and magnesium are also understood to help. Berberine and resveratrol (the good stuff in red wine) may also be of benefit, but have less evidence.
Eat lower glycemic index foods. Glycemic index (GI) is a measure of how quickly the glucose from carbohydrate foods, like sugar and flour, get into the blood stream. The more processed a food is, generally the more quickly it is digested and absorbed, spiking blood sugar quickly and requiring more insulin to handle the sugar. For example, brown rice has a lower GI than the more processed white rice. However, once both are processed into flour, the difference disappears and both become higher glycemic foods.
Avoid added sugar. I probably don’t need to say this, but sugar itself (especially in rapidly absorbed forms, like sugar-sweetened drinks) is a big contributor to insulin resistance. It quickly floods the blood stream with sugar that the pancreas then needs to produce extra insulin to clear away.
Omega-3 fats, contained in fish, nuts and seeds (and their oils), eggs (especially omega-3 enriched) and some vegetables (like spinach and brussels sprouts) can also help reduce insulin resistance.
Apple cider vinegar is also believed to improve insulin resistance. I found an easy-to-make recipe for a drink that’s essentially water with apple cider vinegar, lemon juice, and cinnamon added:
- Apple cider vinegar 15 ml (1 tbsp)
- Lemon juice 15 ml (1 tbsp) or juice of 1/2 lemon
- Cinnamon 2.5 ml (1/2 tsp)
- Sweetener to taste
- Water 250 ml (1 cup)
This formula, of course, can be tailored to your liking. It can be made with cold water or you can use warm water to make a sort of tea. They recommend sipping it through a straw to prevent contact of the acidic liquid with the teeth (which has the potential to erode tooth enamel) but, that being said, colas are more acidic than diluted apple cider vinegar, and sugar itself promotes loss of tooth enamel! (See references below for a link to a video on this!) If you find the mixture too sour tasting, try adding more sweetener (I use erythritol/Swerve) or reducing the amounts of vinegar or lemon juice. The idea is to give you another source of insulin-helping food and amounts of the ingredients are not crucial.
Type 3 Diabetes
And, lastly, insulin resistance may have a connection with Alzheimer’s Disease. Some researchers are even calling it Type 3 Diabetes, where resistance to insulin occurs in the brain, preventing it from clearing away the tangles and plaques associated with Alzheimer’s, and causing death of brain nerve cells. Although researchers say more research is needed, evidence is mounting. Risk of Alzheimer’s is noted to be higher in those with diabetes and insulin resistance.
So, there are many reasons to reduce your sugar intake (essentially the Keto diet!) and to check for (and treat!) insulin resistance before it becomes obvious through development of diabetes or other chronic diseases it puts you at risk for! Diabetes, obesity, heart disease, and other preventable conditions associated with insulin resistance are becoming epidemic, putting our health and our healthcare systems at risk in the future. Are you ready to make the changes needed to prevent this? Talk to your doctor about it at your next visit!
References:
14 Natural Ways to Improve Your Insulin Sensitivity – Healthline
Type 2 diabetes: Exercise later in the day may cut insulin resistance – Medical News Today
The 9 Benefits of Apple Cider Vinegar – Dr. Berg’s Blog
12 Foods That Are Very High in Omega-3 – Healthline
Type 3 Diabetes and It’s Role Implications in Alzheimer’s Disease – International Journal of Molecular Science (National Library of Medicine)
The Gut Microbiota and Inflammation: An Overview — National Library of Medicine
The #1 Worst Drink That Dissolves Your Teeth — Dr. Eric Berg








